ONLINE GUIDE FOR THE PREVENTION OF ADDICTION DISORDERS
BLOG
Editorial Board – Working Group for Combating Addiction Disorders, Belgrade Health Festival
Prof. Dr. Janko Samardžić, Clinical Pharmacologist
Prim. Dr. Oliver Vidojević, Child Psychiatrist
Dr sci. med. Svetlana Vučetić Arsić, Neurologist, Addiction Specialist
July 2025
What is Addiction and How Does It Develop?

Addiction is a condition in which a person can no longer control their need to use a substance (such as alcohol, drugs, or medications) or repeat a behavior (e.g., gambling), even though they know it harms them. Initially, these substances or behaviors trigger pleasant feelings of satisfaction or relaxation. However, over time, the brain becomes accustomed and demands more to achieve the same effect. At the same time, the person struggles to function in their usual social environment, experiencing nervousness, insomnia, restlessness, and other physical symptoms. Eventually, biological changes occur in brain function, particularly in areas responsible for reward, memory, and decision-making. Therefore, addiction is a serious health problem that requires multidisciplinary support from doctors, psychologists, and family.
What Are the Most Common Causes of Addiction?

Addiction usually arises from a combination of genetic, psychological, and social factors. Research shows that people with close relatives who have addictions are at higher risk of developing similar issues. Psychological problems such as anxiety, depression, or childhood trauma often lead individuals to use substances as a way to “escape” unpleasant feelings. Family environment, peer pressure, and substance availability also play a major role. Additionally, the earlier a person starts using, the higher the chances of developing addiction, as the developing brain more easily falls into the vicious cycle of habit and craving. Understanding these causes helps in prevention and early problem recognition.
What Types of Addiction Exist?

Addictions can be divided into chemical (substance dependence) and non-chemical (behavioral addictions), both of which have similar effects on the brain and behavior. While substance addictions are caused by chemical changes in the body, behavioral addictions involve habits that become compulsive and hard to control. Both types require recognition and professional help.
Do All Addictions Share the Same Neurophysiological Mechanism, or Do They Differ?
Addictions, whether chemical or behavioral, largely share a similar neurophysiological mechanism involving the activation of the brain’s reward system, primarily dopamine pathways. Despite different substances or behaviors, they all trigger dopamine release, creating pleasure and motivating repetition. However, there are differences: substances directly alter brain chemistry and can cause physical dependence and withdrawal symptoms, while behavioral addictions mostly lack pronounced physical symptoms and are based on psychological craving and compulsive behavior. Additionally, different addictions may activate specific brain structures or pathways to varying degrees, requiring tailored treatment approaches.
Are There Stages in the Development of Addiction?
The development of addiction typically goes through several stages:
Experimentation – The person tries a substance or behavior out of curiosity or peer pressure.
Occasional use – Gradually becomes more frequent.
Loss of control – Use becomes regular and necessary to avoid discomfort like anxiety or irritability.
Chronic addiction – The brain undergoes lasting changes, with possible relapses.
How to Recognize the Symptoms of Addiction?
Symptoms may be hard to spot immediately, but key signs include:
Strong cravings for the substance or activity.
Increased frequency and quantity of use.
Inability to control usage despite negative consequences.
Neglecting responsibilities, family, and friends.
Mood swings, irritability, or depression when unable to engage in the behavior.
Physical symptoms (sweating, tremors, nausea) upon stopping.
Early recognition is crucial for seeking professional help.
What Are the Physical and Psychological Consequences of Addiction?

Addiction severely impacts health and quality of life.
Physical effects: Organ damage (liver, lungs, heart), sleep disorders, weakened immunity, withdrawal symptoms (sweating, fever, nausea).
Psychological effects: Anxiety, depression, memory loss, emotional instability, aggression, social isolation, and other mental disorders.
These consequences strain relationships, work, and social life, creating a vicious cycle that makes recovery difficult without professional help.
When we talk about the use of alcohol, medications and smoking, people who drink, smoke or excessively use sedative medications are often said to have a 'bad habit'. We know that these bad habits are quite socially acceptable in our region. Where is the line when a bad habit becomes an addiction?

The boundary between a ‘bad habit’ and addiction is often not easily noticeable, because at the beginning such behaviors appear as just a routine or a way to relax. However, the key difference lies in the loss of control and the negative consequences that the person suffers, yet continues to ignore. While a bad habit is something a person can stop or reduce when they want to, addiction involves a strong need, often accompanied by craving and physical symptoms if stopped. Social acceptability, to a significant extent, can make it more difficult to recognize the problem.
How does excessive alcohol consumption affect health?

Excessive alcohol consumption can lead to numerous health problems, including liver damage (cirrhosis), heart disease, high blood pressure, digestive system issues, mental disorders (depression, anxiety), and an increased risk of cancer. In the long term, excessive alcohol consumption always initiates serious family conflicts, sometimes domestic violence, pathological jealousy between partners, child neglect or abuse. Individuals who excessively consume alcohol are prone to workplace disciplinary violations or frequent absenteeism, conflicts at work, or creating general danger through violent behavior or traffic offenses.
What alcohol consumption values are considered socially acceptable?

According to global guidelines, one alcohol unit is defined as 10 milliliters (8 grams) of pure alcohol. Standard drinks contain 1-3 alcohol units. Accepted expert recommendations state that socially acceptable alcohol consumption is considered to be 3-4 alcohol units per day for men (equivalent to 750ml of 4% alcohol beer), or 2-3 alcohol units for women (equivalent to 175ml – a glass of wine).
What are the early signs of alcoholism?

Early signs of alcoholism include increased alcohol tolerance, loss of control over consumption, emotional changes (e.g., irritability), withdrawal from social activities, as well as physical symptoms such as tremors or nausea after sudden cessation of alcohol consumption. Subsequently, neglect of professional, family or partner relationships manifests, along with frequent conflict situations at work and/or in the family, domestic or partner violence. In the psychological domain, alcohol-dependent individuals develop clinical pictures of heightened anxiety, depression, or eating disorders. Women who excessively consumed alcohol during pregnancy risk giving birth to a child with fetal alcohol syndrome.
How is alcohol dependence treated?
Treatment for alcohol dependence usually begins with implementing substance cessation and a detoxification protocol in outpatient or hospital settings. Pharmacotherapy is applied to prevent the occurrence of withdrawal syndrome symptoms, prevent relapse into alcohol consumption, and establish prolonged abstinence. Concurrently, supportive psychotherapy takes place, often utilizing cognitive-behavioral therapy and family therapy during the rehabilitation phase. Group or individual psychotherapy is an integral part of alcohol dependence treatment, and the participation of collaborators in treatment is often necessary and desirable. Additionally, there are self-help groups such as “Alcoholics Anonymous.” An individualized approach is crucial for successful treatment and resocialization of alcohol-dependent individuals.
What is a "blackout"?
A “blackout” refers to a state where a person cannot remember events that occurred during a period of alcohol consumption. This phenomenon occurs due to alcohol’s effect on the brain, particularly the hippocampus, which is responsible for forming new memories. In these twilight states, individuals may commit criminal acts, frequently provoke conflict situations, or engage in self-harm.
What types of drugs exist in general?

Drugs belong to the group of substances collectively called psychoactive substances (PAS). The name indicates the primary property of PAS, which is their effect on the brain. As a consequence of their impact on different brain regions, changes occur in the functioning of the central nervous system (CNS) and the organism as a whole. Based on legal regulations, PAS can be classified into categories of legal substances (alcohol, nicotine, benzodiazepines, methadone, buprenorphine, morphine) and illegal substances (heroin, cocaine, ecstasy, amphetamines, cannabis).
Based on their effects on the brain and the sensations they produce, drugs are classified into stimulants (cocaine, amphetamines), depressants (alcohol, benzodiazepines), hallucinogens (LSD, psilocybin mushrooms), and cannabinoids (marijuana). Cannabinoids form a separate group because cannabis most often acts as a depressant, reducing CNS activity, but in the early stages of consumption, it can induce euphoria and heightened perception, demonstrating its stimulant effects, including accelerated heart rate. Finally, THC (tetrahydrocannabinol), the main psychoactive component of cannabis, can cause perceptual changes, spatial distortion, temporal slowing, and even hallucinations.
Which drugs cause the strongest addiction?

The drugs that cause the strongest addiction include heroin, cocaine, and similarly, nicotine and alcohol. These substances affect neurochemical and structural pathways in the brain regions responsible for the reward process. The same brain regions—the limbic system and associated neural pathways to the cerebral cortex—are responsible for behavioral changes that manifest during drug use. Drugs influence learning, memory, and motivational behaviors, leading to changes in the mental, physical, and social aspects of a person’s personality, which can result in rapid and severe addiction.
How do drugs affect the brain and body?
Drugs act at different levels of our organism. In the brain, they cause changes in neurochemical systems. Addiction affects neurotransmitters, particularly dopamine, which plays a key role in the reward system. The use of drugs or addictive behaviors leads to increased dopamine levels, creating feelings of euphoria or pleasure. Over time, the brain adapts to these changes, which can diminish natural rewards and increase the need for the substance or addictive behavior. Furthermore, drugs cause structural changes in the brain, and after prolonged use, these changes can become permanent or reversible. These changes most often target the brain regions responsible for decision-making, self-control, and emotional reactions. The consequences include impulsive reactions, lack of self-control, and irrational decision-making.
Addiction often involves alterations in cognitive processes, such as decision-making, planning, and risk assessment. Individuals with substance addiction may struggle to recognize the negative consequences of their actions, further complicating the recovery process. In the body, drugs can cause physical changes, including organ damage, alterations in blood pressure, heart rhythm, liver function, lung damage, and blood vessel deterioration.
Does the addictive substance itself directly cause the deterioration of the organism or specific organs?
Yes, addictive substances can directly lead to the deterioration of the organism or specific organs. For example, alcohol can cause liver damage, while heroin can lead to lung and heart function problems. Additionally, the method of drug use (e.g., intravenous injection) can further increase the risk of infections and other health issues. Drugs can also trigger risky behaviors, leading to the transmission of diseases such as HIV or Hepatitis C.
What are the most effective treatments for drug addiction?
The most effective treatments for drug addiction involve a combination of therapies, always tailored to the individual patient. This approach relies on pharmacotherapy, psychotherapy, and social rehabilitation. Depending on the type of substance, different treatment protocols are applied. The beginning of treatment involves the cessation of drug use and a detoxification phase aimed at preventing relapse and alleviating withdrawal symptoms. Treatment can be conducted in outpatient or hospital settings. It includes individual or group therapy, following good clinical practices that also involve the participation of collaborators in the addict’s treatment.
The most commonly applied psychotherapeutic approach is cognitive-behavioral therapy (CBT). Group therapy includes various therapeutic procedures in which family members may participate when family therapy is applied, or it may involve only patients, as in self-help groups like “Alcoholics Anonymous” or “Narcotics Anonymous.” Additionally, there are rehabilitation centers that admit, treat, and rehabilitate addicts following the principles of group therapy combined with work and social integration. Therefore, the most effective treatment for drug addiction requires an individualized approach based on the specific needs of the patient.
What is the "harm reduction" principle, and is it applied in our country?
“Harm reduction” is an approach focused on minimizing the negative consequences of drug use rather than solely emphasizing abstinence. This principle includes programs such as needle exchange, education on HIV and Hepatitis C transmission, and similar initiatives. In some countries, including Serbia, there are initiatives that apply this approach, but its implementation is still limited and often faces social and political challenges.
In a pharmacological sense, harm reduction programs also include the use of opioid substitution therapies, such as methadone and buprenorphine, for opioid addiction. Substitution therapy is essentially a treatment but aims at harm reduction. These medications are used in a controlled manner as a replacement for previously consumed opiates in addicts who cannot achieve full abstinence, frequently relapse, commit crimes, and are at risk of infectious diseases such as HIV and Hepatitis C or B.
Is Smoking Considered an Addiction Disorder?
Consumption of tobacco through smoking cigarettes or cigars is regarded as one of the oldest addictions, accompanying humanity for centuries. Nicotine, the active component of tobacco, causes both physical and psychological dependence. When a person smokes, nicotine quickly enters the bloodstream and reaches the brain, where it activates receptors that release dopamine, a neurotransmitter associated with feelings of pleasure and reward. This addiction can lead to chronic tobacco use despite known health risks, such as heart disease, malignancies, and chronic respiratory illnesses. Smoking is a complex behavioral pattern where, in addition to nicotine—the primary addictive agent—the individual also experiences sensory, ritualistic, and even social aspects tied to tobacco consumption.
How Does Nicotine Affect the Brain, and Is It Responsible for Addiction?

Nicotine is the main cause of tobacco addiction. When a person inhales cigarette smoke, nicotine reaches the brain very quickly (within seconds) and binds to nicotinic acetylcholine receptors. This triggers the release of dopamine, the neurotransmitter responsible for feelings of reward and satisfaction. This creates a mechanism of positive reinforcement—the brain associates smoking with pleasure, stress relief, and improved mood, leading to habit formation and psychological and physical dependence. Over time, the brain reduces its natural dopamine production, forcing the individual to smoke more frequently to maintain the same sensation. This is the classic pattern of addiction.
What Are the Risks and Diseases Caused by Smoking, and Is Nicotine Responsible for Them?

Most of the harmful effects of smoking come from other components of tobacco smoke rather than nicotine itself. Tobacco smoke contains over 7,000 chemicals, many of which are toxic and carcinogenic (tar, benzene, formaldehyde, carbon monoxide, etc.).
Major diseases caused by smoking include:
Cardiovascular diseases: Myocardial infarction, stroke, peripheral vascular disease
Chronic lung diseases: Chronic obstructive pulmonary disease (COPD), emphysema, chronic bronchitis
Cancers: Lung, throat, esophageal, bladder, pancreatic, and other cancers
Reproductive disorders: Infertility, pregnancy complications
Nicotine itself is not the primary cause of these diseases, but it has vasoconstrictive effects, narrowing blood vessels and increasing blood pressure, which contributes to cardiovascular problems. The resulting addiction indirectly leads to prolonged exposure to toxic substances in cigarettes.
Thus, nicotine is responsible for addiction, while other components of tobacco smoke are responsible for organ damage.
Does the Behavior of "Nicotine Addicts" Differ from That of Alcohol or Drug Addicts?
Although nicotine addiction shares the same brain mechanisms (interaction with the reward center), there are behavioral differences between smokers and those addicted to other psychoactive substances. Smokers, while consuming an addictive substance, do not exhibit aggressive behavior, do not cause traffic accidents, and do not engage in actions that endanger themselves or others—unlike those under the influence of alcohol or narcotics.
Similarities:
-
All types of addiction share biological foundations in the brain, primarily through the dopamine reward system.
-
Individuals develop tolerance, experience withdrawal symptoms, and repeatedly use the substance despite harmful consequences.
-
Addicts may exhibit compulsive behavior and a strong psychological craving for the substance.
Differences:
-
Nicotine addiction is often more socially accepted and does not cause visible behavioral changes like alcohol or psychoactive drugs (e.g., aggression, confusion, motor impairment).
-
Smokers function “normally” in daily life, so their addiction is often underestimated. Decades ago, smoking was a socially acceptable habit in many countries.
-
Alcohol and drugs more frequently lead to social dysfunction, family problems, workplace issues, and legal troubles.
-
Nicotine withdrawal symptoms (nervousness, insomnia, irritability) are unpleasant but not life-threatening, unlike withdrawal from alcohol or opioids.
How Is Nicotine Addiction Treated, and Is the Harm Reduction Principle Applicable in This Field?
Treatment for nicotine addiction involves a combination of psychological and pharmacological approaches tailored to the level of dependence, patient motivation, and comorbidities.
-
Psychological Support:
-
Motivational interviewing: Helps individuals find internal motivation to quit.
-
Cognitive-behavioral therapy (CBT): Identifies and modifies smoking-related behavioral patterns.
-
Support groups (e.g., Nicotine Anonymous).
-
-
Pharmacological Therapy:
-
Nicotine Replacement Therapy (NRT): Patches, gum, lozenges, nasal sprays, or inhalers. These provide controlled nicotine doses to alleviate withdrawal symptoms without the harmful chemicals in tobacco smoke.
-
Medications affecting the brain:
-
Bupropion: An antidepressant that reduces nicotine cravings.
-
Varenicline (Champix): A partial nicotine receptor agonist that reduces smoking satisfaction and eases withdrawal.
-
-
Some cases combine multiple methods (e.g., patch + gum + psychotherapy).
-
Harm Reduction in Nicotine Addiction:
Harm reduction is applied cautiously in nicotine dependence treatment. If a person cannot or will not quit nicotine use entirely, the goal shifts to minimizing health risks. Examples include:
-
Smoke-free products:
-
E-cigarettes (vapes): Less harmful than traditional cigarettes because they do not burn tobacco, eliminating tar and carbon monoxide. However, they still contain nicotine and potential irritants. Long-term safety is not fully confirmed. They may serve as a transitional step but are not the first choice in official guidelines.
-
Heated tobacco products (HTPs): Also less toxic than cigarettes since tobacco is heated, not burned. Still contains nicotine and some harmful substances. Controversial because they may sustain addiction and attract younger users.
-
-
Gradual reduction: Some smokers successfully reduce cigarette numbers before quitting completely, though abrupt cessation is more effective.
Conclusion:
The most effective approach is complete smoking cessation with therapy and support. Harm reduction can be a transitional solution but is not a substitute for overcoming nicotine addiction. Nicotine replacement products and medications are safer alternatives and effective in easing the transition away from tobacco smoke.
Which medications are most commonly misused in Serbia?
In Serbia, the most frequently misused medications belong to the benzodiazepine group, which are pharmacologically used as sedatives and anxiolytics. Among them, the most well-known are bromazepam, diazepam, lorazepam, and alprazolam. These drugs are often prescribed for treating anxiety, insomnia, and muscle spasms. However, their prolonged use can lead to the development of tolerance, dependence, and withdrawal symptoms upon abrupt discontinuation. In addition to benzodiazepines, antidepressants—particularly SSRIs (selective serotonin reuptake inhibitors)—are misused, as are opioids such as methadone, hydrocodone, oxycodone, and buprenorphine. There is also misuse of psychostimulants like amphetamine and methylphenidate, which are used to treat attention disorders.
Should a general practitioner prescribe sedative medications on their own initiative, without consulting a psychiatrist?
A general practitioner may, in certain situations, prescribe sedative medications, especially for short-term treatment of mild or transient symptoms of anxiety, stress, or insomnia. However, due to the risk of dependence and adverse effects, it is recommended that such therapy be as brief as possible and that the physician monitors the patient during treatment. In cases where symptoms are more severe, chronic, or recurrent, consultation with a psychiatrist is mandatory. A psychiatrist can provide an accurate diagnosis and recommend appropriate therapy, including other types of medications (such as antidepressants) or psychotherapy.
For which non-psychiatric medical conditions are sedative medications most commonly prescribed, and how great is the risk of developing dependence in such cases?
Sedative medications may also be prescribed for various physical conditions unrelated to mental health, such as chronic pain, cardiac issues, or digestive disorders, as stress and tension can exacerbate symptoms. In such cases, these medications help alleviate symptoms and improve coping mechanisms. However, it is crucial to emphasize that their use should be short-term and strictly supervised by a physician, as prolonged and uncontrolled use can lead to dependence.
To what extent do sedative medications harm users, and to what extent do they help them?
When used correctly, sedative medications can significantly help patients by quickly reducing anxiety, stress, and insomnia, enabling them to better handle difficult situations and improve their quality of life. When used properly, under medical supervision and for short periods, they are effective and relatively safe. However, if used for too long, in high doses, or without control, they can cause side effects such as drowsiness, weakness, memory and concentration problems, as well as dependence. Long-term use can significantly impair daily functioning, so it is important to use these medications cautiously, as prescribed by a doctor, and with additional treatment support when necessary.
To what extent is the misuse of anesthetics present in Serbia, and for what purposes?
In Serbia, there is misuse of certain anesthetics, particularly among younger individuals. The most notable example is ketamine, which is abused for its hallucinogenic and euphoric effects. However, this misuse can lead to serious mental disorders, including psychotic episodes. Another example is nitrous oxide, known as “laughing gas,” which is abused for its immediate euphoric and laughter-inducing effects. Its misuse can cause drops in blood pressure, cardiac arrhythmias, and reduced oxygen levels in the blood, leading to serious health damage. The non-medical use of anesthetics represents a significant public health concern, making it essential to raise awareness about the dangers of misuse and provide proper education and support, especially to young people.
What is polydrug abuse (politoksikomania)?

Polydrug abuse refers to the simultaneous misuse of multiple psychoactive substances. Individuals suffering from polydrug abuse often do not exhibit dependence on just one substance but instead use various drugs to enhance effects or counteract the unwanted symptoms of one drug with another. This practice significantly increases the risk of overdose, serious physical and psychological consequences, and complicates treatment, as therapy must address multiple types of addiction simultaneously. Polydrug abuse is becoming increasingly common and is considered an especially dangerous form of substance use disorder.
How to Recognize Internet Addiction?

Internet addiction is a clinical disorder with strong negative consequences on an individual’s social, professional, family, financial, and economic functioning. It represents a modern form of addiction in which internet use becomes the dominant life activity, isolating the person from other social interactions and creating harmful effects for both the individual and their surroundings. Signs that internet addiction may have developed include:
-
Excessive time spent online (several hours daily, without breaks, at various times of the day).
-
Obsessive focus on digital content, neglecting previous interests and hobbies.
-
Behavioral and emotional changes—children may become irritable, withdrawn, and lose interest in socializing with friends.
-
Physical symptoms—poor posture, fatigue, headaches.
Types of digital addiction include:
-
Information addiction (compulsive, aimless browsing).
-
Gaming addiction (when no other activity brings satisfaction).
-
Social media addiction (constant need to stay online).
What are psychological Effects of Excessive Internet Use & Warning Signs in Children?

Addiction – one of the biggest challenges with online gaming and internet use is developing addiction. Addiction develops from daily use of “something” for several hours. Children may obsessively focus on games and become hard to stop or separate from screens. Excessive and inappropriate internet use can affect their mental, social and emotional abilities.
Social isolation – excessive screen time can lead to social isolation in children. Instead of spending time with other children in real world, children may withdraw into virtual world, which can delay development of crucial social skills important for their emotional, social and mental development.
Inappropriate content – many games contain violent elements. Also, their themes are often age-inappropriate and can negatively affect children’s healthy development. It’s important to explain to children that for their safety, health – both mental and emotional – it’s necessary to block apps that expose them to inappropriate content.
Cyberbullying danger – online games allow interaction with other players, but this carries risks. Children may be insulted and bullied through games and fake gaming profiles. This can affect their health, self-esteem and safety.
Over 750,000 predators are online every second hiding behind fake profiles.
Lack of physical activity – prolonged sitting in front of screens reduces desire for physical activity. Insufficient physical activity affects children’s health leading to obesity, poor fitness, muscle and bone problems.
How Can Internet Addiction Be Reduced? What Can Parents Do?
-
Set time limits—use parental control apps to enforce screen time rules (children struggle with self-regulation due to intentionally addictive game designs).
-
Monitor content—be aware of what children consume online to detect behavioral changes early.
-
Encourage diverse activities—support offline hobbies, sports, and social interactions.
-
Open communication—discuss online risks and encourage children to share concerns.
-
Educate on online safety—teach them to recognize and avoid harmful content.
What Are the Consequences of Uncontrolled Internet Use in Children?
-
Addiction—obsessive focus on games/social media, making it hard to disconnect.
-
Social isolation—withdrawal from real-world interactions, impairing emotional and social development.
-
Exposure to inappropriate content—violent or age-inappropriate material.
-
Cyberbullying risks—online harassment via games or fake profiles.
-
Physical inactivity—leading to obesity, poor posture, and muscle/bone issues.
-
Over 750,000 online predators actively target children through fake profiles.
One aspect of these addictions is excessive gaming, another relates to social media addiction. What is the professional stance - are these real addictions, are they classified as such?
Gaming (video games)
From early childhood, children love playing as it animates, entertains them and represents important interactive activity while also serving social and emotional purposes. As acquired skills develop further, game characteristics become more complex, moving from sensory-motor games to complex symbolic games with precise rules that help refine social skills and human behavior norms. Thus, play is essential for proper child development.
In recent decades, children’s free time increasingly becomes video game time, making it necessary to examine both positive and negative effects on children’s psychosocial development.
Research confirms video games improve:
-
Access to culture and technological thinking
-
Stimulate mental processes (memory, thinking ability)
-
Calculation skills and formulating winning strategies
-
Hand-eye coordination
However, there are also clear negative effects of video games on children and their development:
-
Alienation from reality
-
Lack of empathy, difficulties in social contacts
-
Sedentary lifestyle, passivity and lack of motor activity, especially in live play with other children, adults, pets etc.
-
Excess weight, sedentary lifestyle, reduced physical activity essential for children
-
Excessive sense of power and control related to game content and type, level of aggression in games
-
Vision damage from prolonged screen exposure (computers, mobile phones, tablets etc.)
The strong influence of violent video game content on behavior shouldn’t be ignored – several studies show this content desensitizes the brain to “difficult” images and triggers aggressive behavior in children.
One of the biggest risks of excessive gaming is blurring the line between use and abuse, risking development of actual addiction. Excessive video game use can lead to information overload preventing children from retaining, managing, processing and interpreting the amount of data they’re exposed to. This primarily happens with games and virtual simulations featuring such graphic perfection that they significantly reduce the gap between reality and fiction. Early, intense and prolonged contact makes it hard for children to establish clear boundaries between human and device, living and non-living, fantasy and reality – which is extremely important.
In the internet age, we can’t prevent children from playing video games. On the contrary, to protect them from dangers, it’s necessary to talk with them, listen to them and answer their questions patiently and optimistically. Monitor your child’s behavior and habits and intervene only when necessary – this way you’ll build their trust and empower them, guiding them toward more mature and autonomous growth and development.
The new revision of WHO’s International Classification of Diseases (ICD-11) includes gaming disorder as a diagnosis classified under impulse control disorders. There’s also diagnosis QE22 Hazardous gaming (when consequences are expected in future but not currently present in child’s behavior).
We can speak of addiction when there’s:
-
Strong preoccupation with games
-
Increasing gaming time
-
Loss of control over time spent gaming
-
Strong discontent, agitation, even aggressive behavior when stopped from gaming
This must be accompanied by neglecting negative consequences or hiding time spent gaming.
To avoid all risks associated with excessive video game use, precise rules can be implemented. Parents must maintain control through:
A. Parents should control time children spend gaming to prevent it becoming prolonged daily activity – no more than 2 hours total for school-aged children, especially not in evening before bedtime when increased brain activity and arousal make falling asleep harder, particularly considering child’s age.
B. Breaks during gaming are very important to give cognitive and visual systems rest and reintroduce elements of interaction with environment and reality.
C. Promote gaming in gatherings with friends or relatives to use games as socialization tool rather than isolation.
D. Familiarize yourself with, control and verify content of purchased games according to child’s age and temperament, avoiding violent or extremely competitive challenges.
E. From early age, guide children toward healthy lifestyles – socializing with friends and family, and recreation.
Social media addiction
Children/adolescents spend significant time on social media – practically all their free time, and at night time meant for rest and sleep which is so precious in this developmental period. Social media interferes with their contact with others.
WHO warned last September that problematic social media use is increasing among European children. In 2022, 11% of adolescents (13% girls and 9% boys) showed signs of problematic use, compared to 7% four years earlier. They displayed symptoms similar to addiction symptoms – besides excessive time on computers/phones, neglecting responsibilities. Some youth are online even at night, disrupting their sleep process. Consequently, they’re often sleep-deprived, irritable, quarrelsome, sensitive to criticism and prone to withdrawing from family life – for example eating alone in their room rather than with family.
Regarding excessive social media use - they often promote unrealistic beauty standards, frequently triggering people to undergo uncritical aesthetic procedures or extreme diets to achieve looks promoted on social networks. Is this addiction or another disorder?
Social networks have become key sources of beauty ideals, with influencers often presenting idealized body images (further digitally enhanced, unrealistic). This creates a “body culture” valuing only certain appearances, making those who don’t meet these standards feel inferior.
Also, social media filters often change how we see ourselves and others, distorting reality perception. Unrealistic beauty standards in media profoundly impact mental health. Many feel insecure and dissatisfied with their appearance, potentially leading to eating disorders, anxiety and depression. Those who feel insufficiently attractive often avoid social situations, suffer low self-esteem and may become socially isolated.
Social media’s influence on youth self-confidence is significant since they typically base their self-worth on others’ opinions, making them easily manipulated by malicious individuals.
Promotion of unrealistic beauty standards often leads to discrimination and stigmatization of those not fitting these norms. People not conforming to socially accepted beauty ideals may face bullying and humiliation, particularly harming emotional wellbeing and self-confidence in youth, especially girls.
Research on digital beauty standards’ impact shows:
1/3 of average social media users believe they should lose weight after seeing online images
1 in 8 feel inadequate
6 in 10 teens receive diet advice online (mostly TikTok), contributing to rising eating disorders and body dysmorphia
Frequent exposure to edited model images has established deeply rooted standards for many women
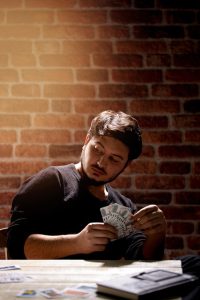
What is gambling in general, and how is a gambler defined?

Pathological gambling is an uncontrollable urge or compulsion that drives a person to persistently continue gambling despite the harmful consequences this behavior causes for themselves, their immediate surroundings, and broader environment. The most widespread form of gambling is betting, which—due to its online accessibility—poses the greatest threat to children and adolescents. In the International Classification of Diseases (ICD), pathological gambling is categorized under “Impulse Control Disorders” (F63.0). It involves specific behavioral disorders characterized by repetitive actions without clear rational motivation, driven instead by impulses the person cannot control. These compulsive behaviors persist despite negative consequences.
In the brain of a gambler, gambling triggers stimulation and a sense of immediate satisfaction and reward, similar to the effects of drugs or alcohol, which over time leads to gambling addiction.
A gambler is a person under the strong influence of pathological gambling impulses. They compulsively repeat gambling-related behaviors (such as betting) and are willing to risk things they value in pursuit of an illusory win. Gamblers fail to recognize the consequences and complications of their compulsive and repetitive behavior—family problems, financial ruin, health deterioration, and other issues that worsen over time.
In children and adolescents, gambling leads to sleep disturbances, poor concentration, attention deficits, and memory problems, resulting in declining academic performance and even school dropout. Gambling always negatively impacts the entire family, as it requires constant financial investment, often at the family’s expense, deeply damaging relationships and affecting even those not directly involved in the gambling.
How to recognize gambling addiction?
Signs and symptoms of compulsive gambling include:
-
Complete preoccupation with gambling—constantly planning how to obtain more money to continue gambling.
-
Intense excitement when dealing with large sums of money or potential gambling rewards.
-
Repeated unsuccessful attempts to control, reduce, or stop gambling.
-
Nervousness, agitation, and irritability when access to gambling is restricted or removed.
-
Using gambling as an escape from problems or to alleviate negative emotions (e.g., helplessness, guilt, anxiety, depression).
-
Persistent attempts to recover losses through further gambling (known as “chasing losses”).
-
Lying and deceiving family members or close friends to hide the extent of gambling.
-
Endangering or losing important relationships (family, friends) or broader social connections (school, peer groups, sports clubs, etc.).
-
Resorting to theft, fraud, or antisocial actions in extreme situations to obtain money for gambling.
-
Compulsive repetition of destructive behavior patterns, which can lead to depression, self-destructive tendencies, insomnia, nervousness, irritability, and increased risk of alcohol or substance abuse.
What are the consequences of gambling addiction?
Pathological gambling negatively affects both the gambler’s physical and mental health, as well as the well-being of their family members. Physical issues in gambling addicts are often stress-related, including:
-
Insomnia
-
Headaches
-
Increased nervousness
-
Poor attention and concentration
-
Memory decline
-
Loss of motivation and interest in previous activities
-
High blood pressure
Alcohol and substance abuse are highly prevalent among gambling addicts (occurring in 60% of cases), with all the associated risks. Depression is the most common psychiatric disorder in gamblers, and self-destructive tendencies may also emerge.
Family consequences often include:
-
Early detachment from family
-
Frequent arguments and physical violence
-
Prolonged absences from home
-
Neglect of family responsibilities
-
Secretive and manipulative behavior
-
Theft of money or valuables from the household
-
Emotional withdrawal and inconsistency
-
Domestic violence (in severe cases, gamblers may coerce family members into providing money)
For children and adolescents, the most common social consequence is school dropout (drop-out), with long-term negative effects on their future.
What are the strategies for preventing and treating gambling addiction?
The psychological nature of gambling addiction, combined with persistent denial, indicates that the root issue lies within the gambler’s personality rather than gambling itself. Immaturity, emotional emptiness, social decline, indifference, and pathological lying isolate the gambler, leading to social marginalization—a dynamic that often extends to the entire family.
Gamblers typically resist treatment, feeling unprepared and unmotivated to quit. They associate stopping gambling with a loss of freedom and life satisfaction, perceiving external intervention as excessive control. While gambling, they feel powerful and in control—only the consequences of gambling trouble them, which they wish would resolve on their own so they could continue gambling “more wisely.”
Motivating a gambler to seek treatment requires confrontation, where problems are clearly outlined without moralizing (which is counterproductive). In motivational interviews, emphasis should be placed on:
Helping the gambler gain insight into their problem.
Strengthening the healthy part of their personality to control the addictive behavior.
Clarifying that they are an addict, that their environment is suffering, and that recovery depends on their commitment to complete abstinence.
Counseling and brief interventions are useful for families seeking help for their children. Family involvement is crucial throughout treatment, with continuous support, psychoeducation, and a strong therapeutic alliance.
In severe cases (with frequent relapses), psychiatric treatment may include:
Day hospitals for partial hospitalization (family treatment while continuing school/work).
Outpatient treatment and monitoring (minimum 12 months).
Group and family therapy (3–12 months).
Additional treatment forms, especially when comorbid conditions exist (alcoholism, substance abuse, depression, suicidal tendencies, etc.).
Preventive measures for parents and families dealing with youth gambling problems:
Spend quality time with your children.
Encourage involvement in sports, creative activities, socializing, or constructive hobbies.
Discuss the risks of gambling openly.
Be aware of their social circle and its influence.
Set clear boundaries/rules and define consequences for breaking them.
Remember: Gambling is NOT a socially permitted activity for those under 18!
References
1. Rösner S, Petzold MB, et al. Classification of psychoactive substances) Der Nervenarzt, Springer Verlag, 2020
DOI: 10.1007/s00115-020-00928-3
2. Baumann MH, Solis E Jr, Wiley JL, et al. Baumann MH, Solis E Jr, Wiley JL, et al. Neuropharmacology of New Psychoactive Substances.Neuropharmacology,2021
DOI: 10.1016/j.neuropharm.2020.108168
3. Republic og Serbia, Ministry of Health. National drug situtation overwiev; 2022.
4. Sher L, Vilens A. Handbook of Substance Misuse and Addictions. Springer Nature, 2022.
17. EUDA (2025): European Drug Report 2025 Harm reduction (European Drug Report 2025)
18. DPNSEE/UNODC (2023): Launching the project in Serbia
22. Gao C. et al.Alcohol consumption and its association with cancer, cardiovascular, liver and brain diseases: a systematic review of Mendelian randomization studies.Fron Epidemiol, 2024.
DOI: 10.3389/fepid.2024.1385064
23. World Health Organization (WHO).Tobacco: Key Facts.2025.Geneva.
25. WHO global report on trends in prevalence of tobacco use 2000-2030. WHO, Geneva, 2024
26. National Institute on Drug Abuse (NIDA).Is nicotine addictive?
29. 2018 ACC Decision Pathway on Tobacco Cessation Treatment – American College of Cardiology
Copyright 2025 © Festival Zdravlja. Izrada sajta: digital-nomad.rs
